Can PTS be prevented?
Although anticoagulant drugs may help to prevent Post-Thrombotic Syndrome (PTS) by reducing the risk of recurrent DVT and/or reducing inflammation, PTS develops frequently despite the use of these medications (1,2,3,4). Studies differ on whether clot removal with CDT or PCDT can prevent PTS; the largest, most rigorous ATTRACT Study found that it did not.
Can PTS be Treated?
PTS is difficult to treat effectively. Treatments that are often used include:
- Elastic Compression Stockings;
- Devices that improve circulation in the leg called intermittent pneumatic compression or portable venous return assist devices;
- Supervised exercise programs; and
- Use of “venoactive” medications to improve blood flow.
Published care guidelines do not strongly recommend these therapies as being reliably effective. Basically, because the risk of harm is low, it is worth trying these conservative treatments but the long-term benefit may be limited (14).
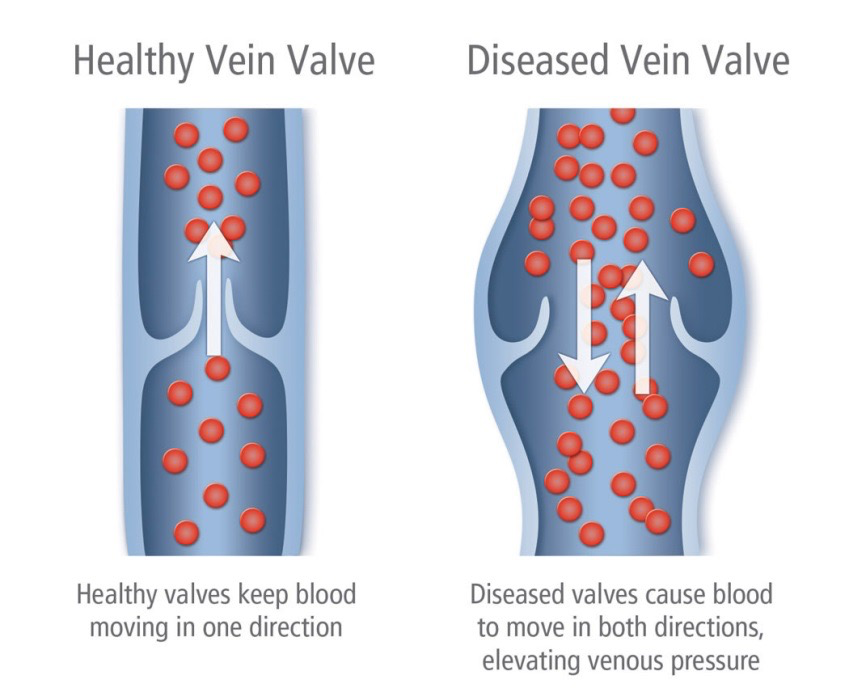
In some cases, a more aggressive approach may be considered to treat PTS. To manage moderate-to-severe PTS symptoms or venous ulcers, patients may consider catheter-directed endovascular therapy (“EVT”) procedures to treat the narrowing or blockage of the blood flow through the large leg veins (“iliac vein obstruction”) and/or back flow (“reflux”) of blood due to leaky vein valves. These procedures have shown promising early results, but their long-term benefits and risks have not yet been clearly established in large, well-designed studies. The C-TRACT Study we are conducting was designed to answer these important questions.
EVT procedures for treatment of moderate-to-severe PTS include:
Stent Placement: A stent is a metal mesh tube that expands and props open a blood vessel. Although there is currently no FDA-approved venous stent, available stents have been used to treat iliac vein obstruction after catheter directed therapy or surgical removal of a clot for acute DVT (5, 15-21). In preliminary studies, stent placement in PTS patients with chronically occluded iliac veins has been associated with reduced obstructive venous physiology, healing of ulcers, and relief of symptoms (22-37).
Endovenous Ablation: Ablation refers to the catheter-directed delivery of heat, medications (causing shrinkage), or adhesive materials into a superficial vein with the intent of causing irreversible occlusion – thus eliminating valvular reflux. This 30-60 minute outpatient procedure may help to reduce venous pressure in the leg with PTS, improving symptoms.
Learn more about opportunities to participate in research trying to determine whether endovascular procedures reduce PTS severity and improve quality of life.
- Baldwin MJ, Moore M, Rudarakanchana N, Gohel M, Davies AH. Post-thrombotic syndrome: a clinical review. J Thromb Haemost 2013; 11:795-805.
- Kahn SR, Shrier I, Julian JA, Ducruet T, Arsenault L, Miron M, Roussin A, Desmarais S, Joyal F, Kassis J, Solymoss S, Desjardins L, Lamping DL, Johri M, Ginsberg JS. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med 2008; 149:698-707.
- Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Huisman, M, King CS, Morris T, Sood N, Stevens SM, Vintch JRE, Wells P, Woller SC, Moores CL. Antithrombotic Therapy for VTE Disease: CHEST Guideline. CHEST 2016, doi: 10.1016/j.chest.2015.11.026.
- Hull RD, Liang J, Townshend G. Long-term low-molecular-weight heparin and the post-thrombotic syndrome: a systematic review. Am J Med 2011; 124:756-765.
- Enden T, Haig Y, Klow N, et al. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial. Lancet 2012; 379(9810):31-38.
- Wysokinska EM, Sobande F, wynsokinski WE, et al. Iliac vein thrombosis: feasibility assessment of randomized controlled trials of endovascular pharmacomechanical thrombolysis. J Thromb Haemost 2010; 8(9):1943-1949.
- Klein SJ, Gasparis AP, Virvilis D, Ferretti JA, Labropoulos N. Prospective determination of candidates for thrombolysis in patients with acute proximal deep vein thrombosis. J Vasc Surg 2010; 51(4):908-912.
- Frulla M, Marchiori A, Sartor D, Mosena L, Tormene D, Concolato A, Hartman L, Prandoni P. Elastic stockings, hydroxyehtylrutosides, or both for the treatment of post-thrombotic syndrome. Thromb Haemost 2005; 93:183-185.
- Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med 2001; 161(17):2105-2109.
- Cohen JM, Akl EA, Kahn SR. Pharmacologic and compression therapies for postthrombotic syndrome: a systematic review of randomized controlled trials. Chest 2012; 141(2):308-320.
- Ginsberg JS, Magier D, McKinnon B, Hirsh J. Intermittent compression units for severe post phlebitic syndrome: a randomized crossover study. CMAJ 1999; 160:1303-1306.
- O’Donnell MJ, McRae S, Kahn SR, Julian JA, Kearon C, MacKinnon B, Magier D, Strulovich C, Lyons T, Robinson S, Hirsh J, Ginsberg JS. Evaluation of a venous-return assist device to treat severe post-thrombotic syndrome (VENOPTS) – a randomized controlled trial. Thromb Haemost 2008; 99:623-629.
- Kahn SR, Shrier I, Shapiro S, Houweling AH, Hirsch AM, Reid RD, Kearon C, Rabhi K, Rodger MA, Kovacs MJ, Anderson DR, Wells PS. Six-month exercise training program to treat post-thrombotic syndrome: a randomized controlled two-centre trial. CMAJ 2011; 183(1):37-44.
- Kahn SR, Comerota AJ, Cushman M, Evans NS, Ginsberg JS, Goldenberg NA, Gupta DK, Prandoni P, Vedantham S, Walsh E, Weitz JI. The post-thrombotic syndrome: evidence-based prevention, diagnosis, and treatment strategies – a scientific statement from the American Heart Association. Circulation 2014; 130(18):1636-1661. PMID 25246013
- Haig Y, Enden T, Slagsvold CE, et al. Determinants of early and long-term efficacy of catheter-directed thrombolysis in proximal deep vein thrombosis. J Vasc Interv Radiol 2012; 24(1):17-24.
- O’Sullivan GJ, Semba CP, Bittner CA, et al. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol 2000; 11(7):823-836.
- Mickley V, Schwagierek R, Rilinger N, Gorich J, Sunder-Plassman L. Left iliac venous thrombosis caused by venous spur: treatment with thrombectomy and stent implantation. J Vasc Surg 1998; 28:492-497.
- Semba CP, Dake MD. Iliofemoral deep venous thrombosis: aggressive therapy with catheter-directed thrombolysis. Radiology 1994; 191:487-494.
- Vedantham S, Sista AK, Klein SJ, Nayak L, Razavi MK, Kalva SP, Saad WE, Dariushnia S, Caplin DM, Chao C, Ganguli S, Walker TG, Nikolic B; for Society of Interventional Radiology and Cardiovascular and Interventional Radiological Society of Europe Standards of Practice Committees. Quality improvement guidelines for the treatment of lower-extremity deep vein thrombosis with use of endovascular thrombus removal. J Vasc Interv Radiol 2014; 25:1317-25. PMID 25000825
- Mewissen MW, Seabrook GR, Meissner MH, et al. Catheter-directed thrombolysis for lower extremity deep venous thrombosis: report of a national multicenter registry. Radiology 1999; 211:39-49.
- Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, Jenkins JS, Kline JA, Michaels AD, Thistlethwaite P, Vedantham S, White RJ, Zierler BK. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 2011; 123(16):1788-1830.
- Nazarian GK, Bjarnason H, Dietz CA, Bernadas CA, Hunter DW. Iliofemoral venous stenoses: effectiveness of treatment with metallic endovascular stents. Radiology 1996; 200:193-199.
- Razavi MK, Hansch EC, Kee ST, Sze DY, Semba CP, Dake MD. Chronically occluded inferior venae cavae: endovascular treatment. Radiology 2000; 214:133-138.
- Blattler W, Blattler IK. Relief of obstructive pelvic venous symptoms with endoluminal stenting. J Vasc Surg 1999; 29:484-488.
- Hartung O, Benmiloud F, Barthelemy P, et al. Late results of surgical venous thrombectomy with iliocaval stenting. J Vasc Surg 2008; 47:381-387.
- Hartung O, Loundou AD, Barthelemy P, et al. Endovascular management of chronic disabling ilio-caval obstructive lesions: long-term results. Eur J Vasc Endovasc Surg 2009; 38:118-124.
- Vogel D, Comerota AJ, Al-Jabouri M, Assi ZI. Common femoral endovenectomy with iliocaval endoluminal recanalization improves symptoms and quality of life in patients with postthrombovic iliofemoral obstruction. J Vasc Surg 2012; 55(1):129-35.
- Rosales A, Sandbaek G, Jorgensen JJ. Stenting for chronic post-thrombotic vena cava and iliofemoral venous occlusions: mid-term patency and clinical outcome. Eur J Vasc Endovasc Surg 2010; 40(2):234-240.
- Hartung O, Otero A, Boufi M, Decaridi G, Barthelemy P, Juhan C, Alimi YS. Mid-term results of endovascular treatment for symptomatic chronic nonmalignant iliocaval venous occlusive disease. J Vasc Surg 2005; 42:1138-1144.
- Neglen P, Hollis KC, Olivier J, Raju S. Stenting of the venous outflow in chronic venous disease: long-term stent-related outcome, clinical, and hemodynamic result. J Vasc Surg 2007; 46:979-990.
- Sarici IS, Yanar F, Agcaoglu O, Ucar A, Poyanli A, Cakir S, Aksoy SM, Kurtoglu M. Our early experience with iliofemoral vein stenting in patients with post-thrombotic syndrome. Phlebology 2013; 1-6.
- Te Riele WW, Overtoom TTC, van den Berg JC, van de Paroordt EDWM, de Vries JPM. Endovascular recanalization of chronic long-segment occlusions of the inferior vena cava: midterm results. J Endovasc Ther 2006; 13:249-253.
- Delis KT, Bjarnason H, Wennberg PW, Rooke TW, Gloviczki P. Successful iliac vein and inferior vena cava stenting ameliorates venous claudication and improves venous outflow, calf muscle pump function, and clinical status in post-thrombotic syndrome. Ann Surg 2007; 245:130-139.
- Alhalbouni S, Hingorani A, Shiferson A, Gopal K, Jung D, Novak D, Marks N, Asher E. Iliac-femoral venous stenting for lower extremity venous stasis symptoms. Ann Vasc Surg 2012; 26:185-189.
- Wahlgren C, Wahlberg E, Olofsson P. Endovascular treatment in postthrombotic syndrome. Vasc Endovasc Surg 2013; 44(5):356-360.
- Kurklinsky AK, Bjarnason H, Friese JL, Wysonkinski WE, McBane R, Misselt A, Moller SM, Gloviczki P. Outcomes of venoplasty with stent placement for chronic thrombosis of the iliac and femoral veins: single-center experience. J Vasc Interv Radiol 2012; 23:1009-1015.
- Catarinella FS, Nieman FHM, de Wolf MAF, Wittens CHA. Short-term follow-up of quality-of-life in interventionally treated patients with post-thrombotic syndrome after deep venous occlusion. Phlebology 2014; 29:104-111.
- Nicolini P; the Closure Group. Treatment of primary varicose veins by endovenousobliteration with VNUS Closure System: results of a prospective multicentre study. Eur J Vasc Endovas Surg 2005; 29:433-439.
- Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, Sessa C, Schuller-Petrovic S. Prospective randomized study of endovenous radiofrequency obliteration (Closure) versus ligation and vein stripping (EVOLVEeS): two-year follow-up. Eur J Vasc Endovasc Surg 2005; 29:67-73.
- Min RJ, Khilnani N, Zimmet SE. Endovenous laser treatment of saphenous vein reflux: long-term results. J Vasc Interv Radiol 2003; 14:991-996.
- Todd III KL, Wright DI, VANISH-2 Investigator Group. The VANISH-2 study: a randomized, blinded, multicenter study to evaluate the efficacy and safety of polidocanol endovenous microfoam 0.5% and 1.0% compared with placebo for the treatment of saphenofemoral junction incompetence. Phlebology 2014; 29(9):608-618.
- Morrison N, Gibson K, McEnroe S, Goldman M, King T, Weiss R, Cher D, Jones A. Randomized trial comparing cyanoacrylate embolization and radiofrequency ablation for incompetent great saphenous veins (VeClose). J Vasc Surg 2015; 61(4):985-994.
- Bootun R, Lane T, Dharmarajah B, Lim CS, Najem M, Renton S, Sritharan K, Davies AH. Intra-procedural pain score in a randomized controlled trial comparing mechanicochemical ablation to radiofrequency ablation: the multicentre Venefit versus Clarivein for varicose veins trial. Phlebology 2016; 31(1):61-65.
- Neglen P, Hollis KC, Raju S. Combined saphenous ablation and iliac stent placement for complex severe chronic venous disease. J Vasc Surg 2006; 44(4):828-833.
- Nayak L, Hildebolt CF, Vedantham S. Post-thrombotic syndrome: feasibility of a strategy of imaging-guided endovascular intervention. J Vasc Interv Radiol 2012; 23(9):1165